Breast cancer is the most common female malignant tumor in the world, with an estimated incidence of 268600 cases in 2019. Recent studies have shown that breast cancer and cardiovascular disease have several common risk factors, which can be changed. It is believed that about 80% of cardiovascular diseases can be prevented by changing risk factors, including current smoking habits, obesity, poor healthy diet scores, poor physical activity, hypercholesterolemia, hypertension and diabetes.
More and more evidence shows that most of the associations between cardiovascular risk factors and breast cancer have common biology, which may provide space for better prevention, early detection and safer treatment strategies (including lifestyle change and preventive treatment).
Considering the interaction of cardiovascular risk factors, the combination of cardiovascular risk factors may convey more information than a single factor. The clinical impact of cardiovascular risk factor aggregation on the incidence rate of breast cancer is still unknown. In addition, it is not clear whether the relationship between cardiovascular risk factors and breast cancer risk can be changed by race / ethnicity and menopausal status.
To address this knowledge gap, this study used data from the community atherosclerosis risk (ARIC) study to conduct a secondary analysis to explore the relationship between the independent and combined effects of cardiovascular risk factors and breast cancer in American women, and to assess the association of risk factors across racial / ethnic groups and menopausal status.
Patient characteristics
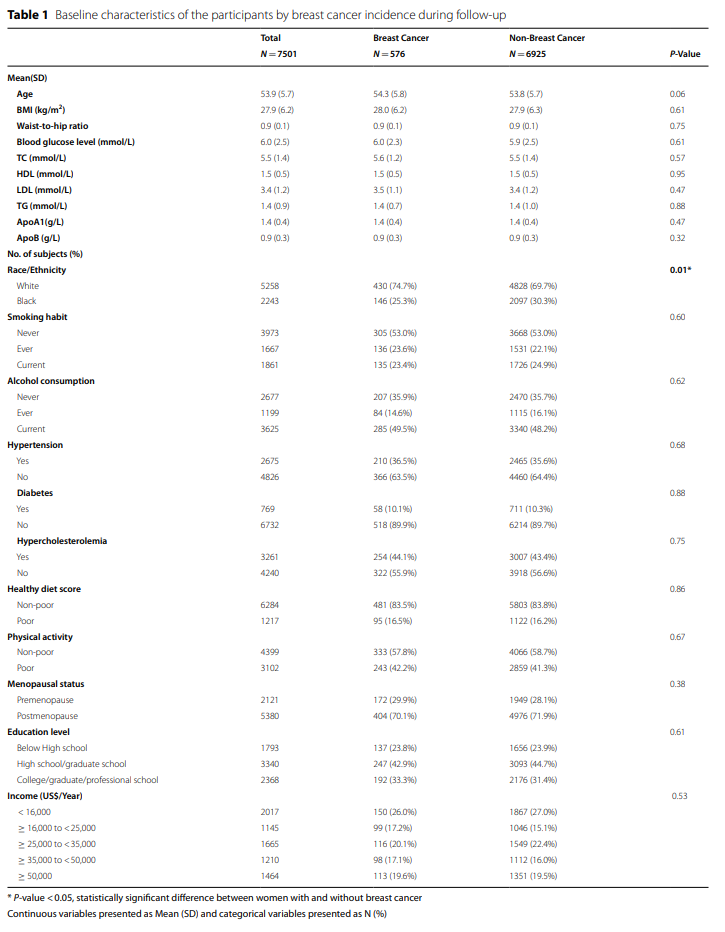
A total of 7501 women were included in this study. The baseline characteristics of incidence rate stratification of breast cancer during follow-up are shown in Table 1. In this study cohort, 576 women were diagnosed with breast cancer (430 white and 146 black). Compared with women without breast cancer, white women were more likely to develop breast cancer than black women (P = 0.01). There was no difference between cases and non cases in baseline age, BMI, smoking habits, drinking habits, menopausal status, education level, income, healthy diet score and physical activity or prevalence of hypertension, diabetes and hypercholesterolemia. In addition, there were no significant differences in blood glucose and serum lipid levels between women with and without breast cancer.
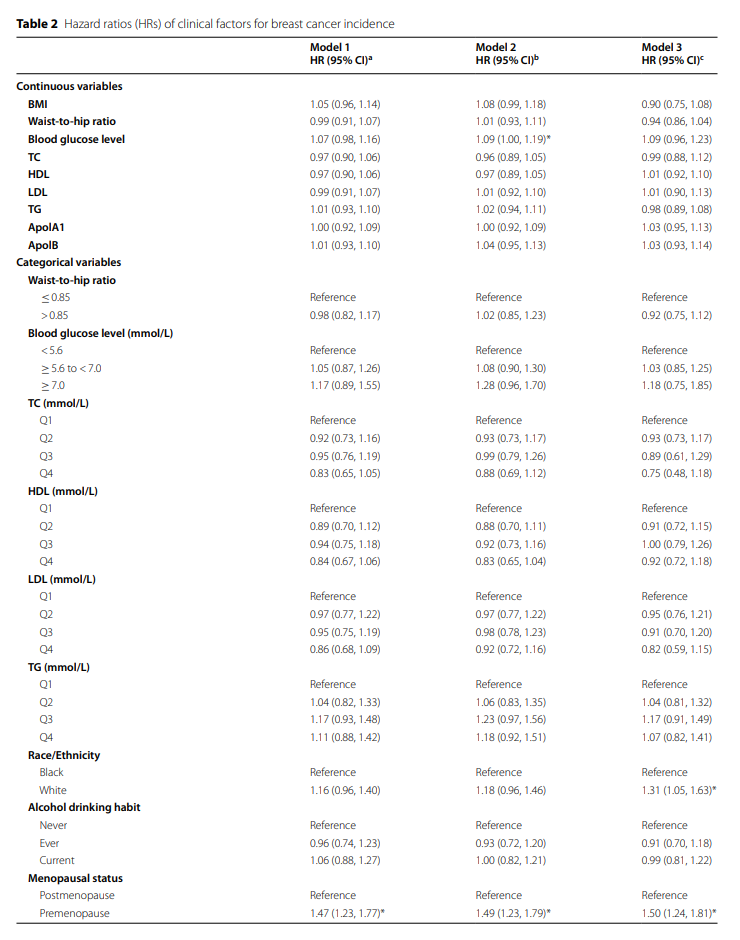
After a maximum follow-up of 26.1 years, with an average of 19.7 ± 6.7 years, 576 cases of breast cancer were reported (incidence rate = 3.9/1000 person years). Table 2 shows the association between clinical factors in the incidence rate of breast cancer. Overall, only white women (HR 1.31, 95% CI 1.05 – 1.63) and premenopausal women (HR 1.50, 95% CI 1.24 – 1.81) were associated with an increased risk of breast cancer after adjusting for multiple factors. In unadjusted or adjusted models, no significant association was observed between serum lipid or glucose levels and breast cancer. In addition, education level and income were not significantly associated with the incidence rate of breast cancer.

Individual cardiovascular risk factors and incidence rate of breast cancer
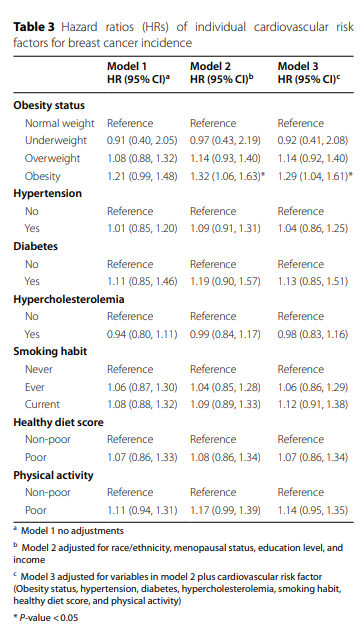
Table 3 summarizes the HR for the diagnosis of breast cancer in women with different cardiovascular risk factors. Obese women were more likely to develop breast cancer than normal weight women (adjusted HR 1.29, 95% CI 1.04-1.61). However, other cardiovascular risk factors: smoking habit, hypertension, diabetes, hypercholesterolemia, poor healthy diet score and poor physical activity were not independently associated with age, race, menopausal status, education level or income adjustment or further multivariable adjusted breast cancer cancer incidence rate.
Combined cardiovascular risk factors and incidence rate of breast cancer
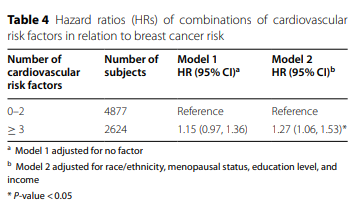
A graphical representation of breast cancer risk stratified by the number of cardiovascular risk factors is shown in Figure 2. In subjects with three or more cardiovascular risk factors, the cumulative risk curve for breast cancer continued to differentiate during follow-up. Figure 3 shows the dose-response relationship between the number of cardiovascular risk factors and the incidence rate of breast cancer, indicating that the HR value increases with the increase of the number of cardiovascular risk factors. Table 4 shows the relationship between combined cardiovascular risk factors and the incidence rate of breast cancer. Women with at least three cardiovascular risk factors had a higher risk of breast cancer than women with fewer than three risk factors. (unadjusted HR 1.15, 95% CI 0.97-1.36; adjusted HR 1.27, 95% CI 1.06-1.53).


Hierarchical analysis of cardiovascular risk factors in incidence rate of breast cancer
Considering that race / ethnicity and menopausal status may affect the incidence rate of breast cancer, the individual cardiovascular risk factors for the incidence rate of breast cancer were stratified (Table 5). Among the individual cardiovascular risk factors, there was a significant correlation between obesity and breast cancer risk in postmenopausal white women (HR 1.49, 95% CI 1.11-2.01), while there was a negative correlation between overweight black postmenopausal women and breast cancer risk (HR 0.44, 95% CI 0.24-0.78). In addition, among postmenopausal black women, current smokers had a higher risk of breast cancer than nonsmokers (HR 1.88, 95% CI 1.19-2.96). In addition, women with poor healthy diet scores had a higher risk of breast cancer (hazard ratio 1.61, 95% confidence interval 1.02-2.54). However, no correlation with other individual cardiovascular risk factors was observed in the stratified analysis.

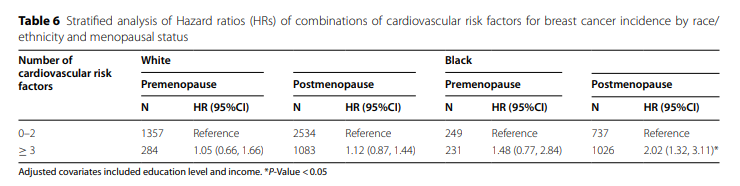
The relationship between breast cancer and cardiovascular risk factors by race / ethnicity and menopausal status is shown in Table 6. Among black women, postmenopausal women with at least three cardiovascular risk factors (HR 2.02, 95% CI 1.32 – 3.11) remained significantly associated, but women with fewer than three cardiovascular risk factors were not significantly associated with breast cancer risk. In addition, the combination of cardiovascular risk factors was not associated with any breast cancer risk in premenopausal black women. In addition, no significant association between combined cardiovascular risk factors and breast cancer incidence rate was observed in premenopausal white and postmenopausal women. In addition, surprisingly, postmenopausal women (2109/5380, 39.2%) or black women (678/2243, 50.0%) had a higher incidence of three or more cardiovascular risk factors than all premenopausal women (515/2121, 24.3%) or white women (1367/5258, 26.0%).
The new findings of this study show that among the participants in the ARIC study cohort, the combination of cardiovascular risk factors is associated with an increased risk of breast cancer, while the impact of a single cardiovascular risk factor is limited to obesity. Women with cardiovascular risk factors ≥ 3 had a 27% increased risk of breast cancer, especially among black postmenopausal women in the United States. From the perspective of public health, combined interventions aimed at changing cardiovascular risk factors can be used to prevent breast cancer in these high-risk groups.
Original source:
Zeng X, Jiang S, Ruan S, et al. Cardiovascular risk factors and breast cancer incidence in a large middle-aged cohort study. BMC Cancer. 2022; 22(1):534. Published 2022 May 12. doi:10.1186/s12885-022-09604-2.
Article source: