High body mass index (BMI) indicates overweight or obesity, which is one of the five major risk factors in the global disease burden study in 2017, causing an estimated 4million deaths each year. Although its prevalence continues to increase in most parts of the world, to date, about 39% and 12% of the world's population can be considered overweight (BMI ≥ 25 kg / m2) or obese (BMI ≥ 30 kg / m2), respectively. In the context of adverse health outcomes associated with BMI, the link between excess body fat and cancer development has been well established. Studies have also reported a dose-response relationship between high BMI life span and cancer risk.

In addition, overweight and obesity are associated with overall mortality and cancer mortality. The most common obesity related malignancies are breast cancer and colorectal cancer. However, the role of BMI in cancer survival and its underlying mechanisms have not been fully elucidated. In order to assess the impact of BMI and cardiac metabolic disease (CMD) on cancer survival, and to investigate the importance of these risk factors in the context of the continuing obesity epidemic, it is important to understand whether BMI and CMD are independently related or mutually reinforcing with cancer survival. Therefore, the aim of this study was to quantify the impact of pre cancer cumulative BMI and cardiac metabolic diseases (including CVD and T2D) on the survival of patients with breast cancer and colorectal cancer, and to investigate the dependence of these risk factors.
The European prospective survey on cancer and nutrition (EPIC) is a cohort study involving 519978 volunteers recruited from 23 centers in 10 countries between 1992 and 2000. In this epic study, repeated BMI assessments of cancer-free participants from four European countries were used to estimate individual BMI trajectories that reflect the predicted mean BMI between the ages of 20 and 50 using a growth curve model. Subjects who developed colorectal cancer or breast cancer after the age of 50 were included in the survival analysis to study the prognostic effects of pre cancer mean BMI and CMD. CMD is defined as one or more chronic diseases in stroke, myocardial infarction and type 2 diabetes.
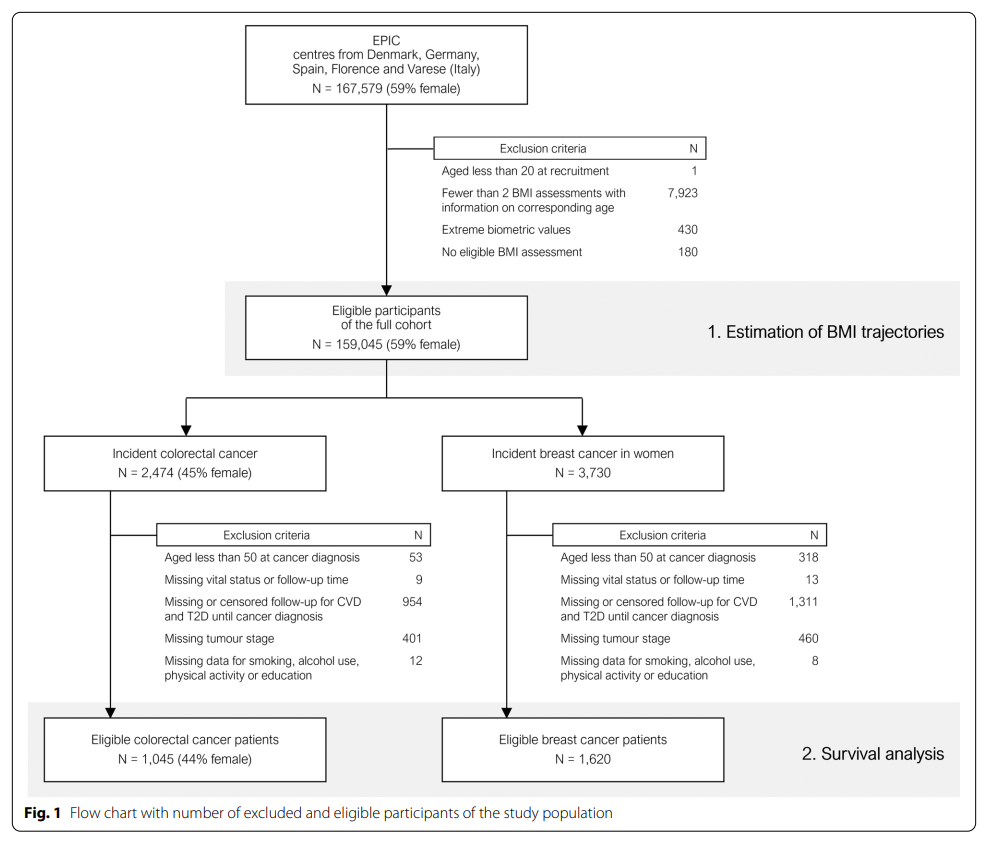
The number of individuals in each phase of the study is shown in Figure 1. A total of 159045 participants contributed an average of 2.4 BMI assessments to the BMI trajectory estimates. In the entire cohort, the predicted mean BMI IQR between the ages of 20 and 50 years was 22.8-26.7 kg/m2, the median for women was 23.9 kg/m2, and the median for men was 25.4 kg/m2.
The study included 1620 patients with breast cancer and 1045 patients with colorectal cancer. The median follow-up time was 9.48 years (IQR 5.42-12.50). 377 patients with breast cancer and 509 patients with colorectal cancer died. See Table 1 for tumor site-specific characteristics and mortality of the study population.
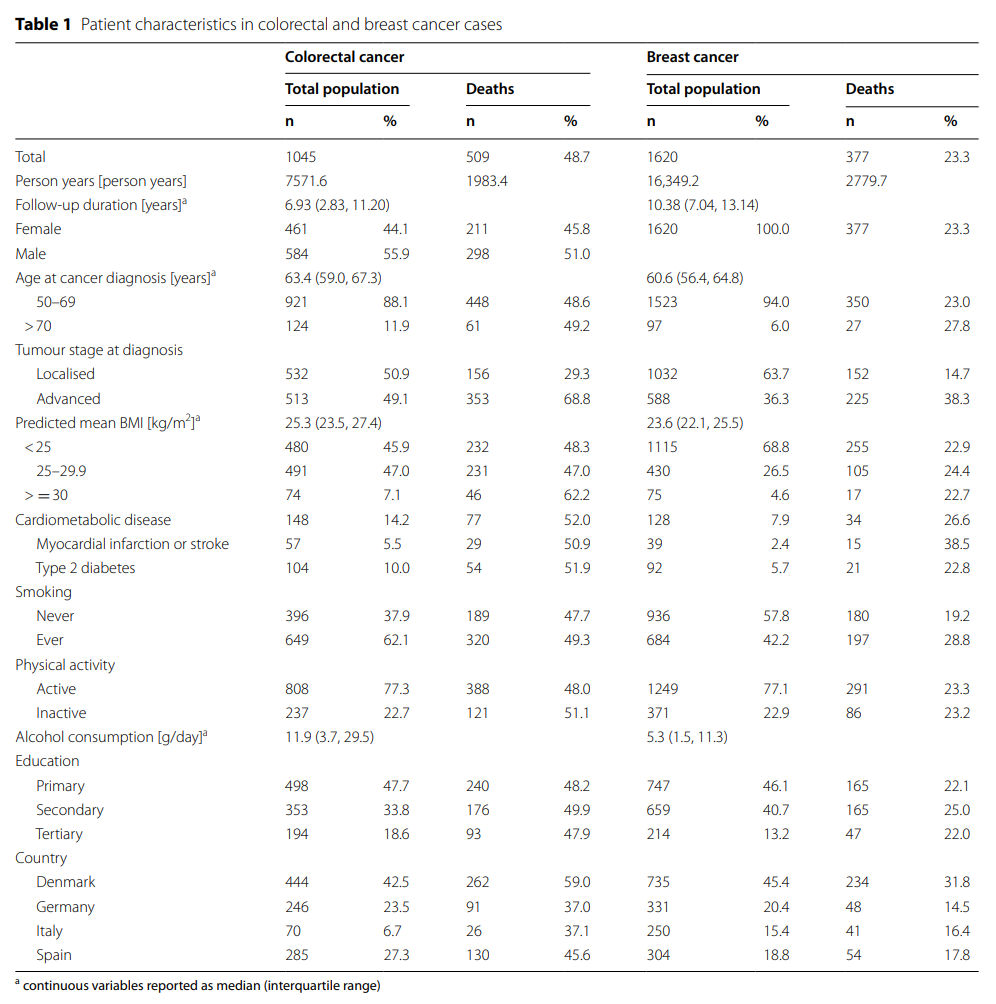
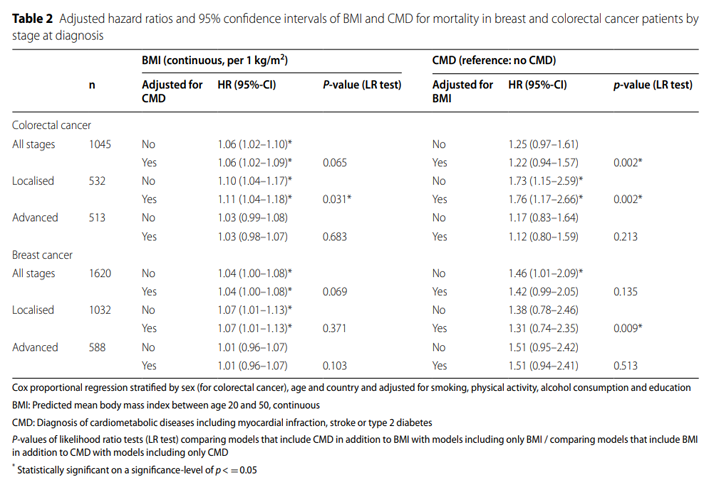
colorectal cancer
According to multivariable adjusted survival analysis, higher mean BMI (per 1 kg/m2 increase) was associated with a 6% increased risk of death in patients with colorectal cancer (Table 2, figure 2). Results there were different stages of the disease at the time of diagnosis.
Higher mean BMI was associated with a 10-11% increase in mortality from localized colorectal cancer (95%ci for HR, 1.04-1.17). The correlation between BMI and late disease survival was less significant (HR 1.03, 95% CI 0.99 – 1.08). After additional adjustment of CMD, the estimated value and confidence interval of BMI effect remained similar.
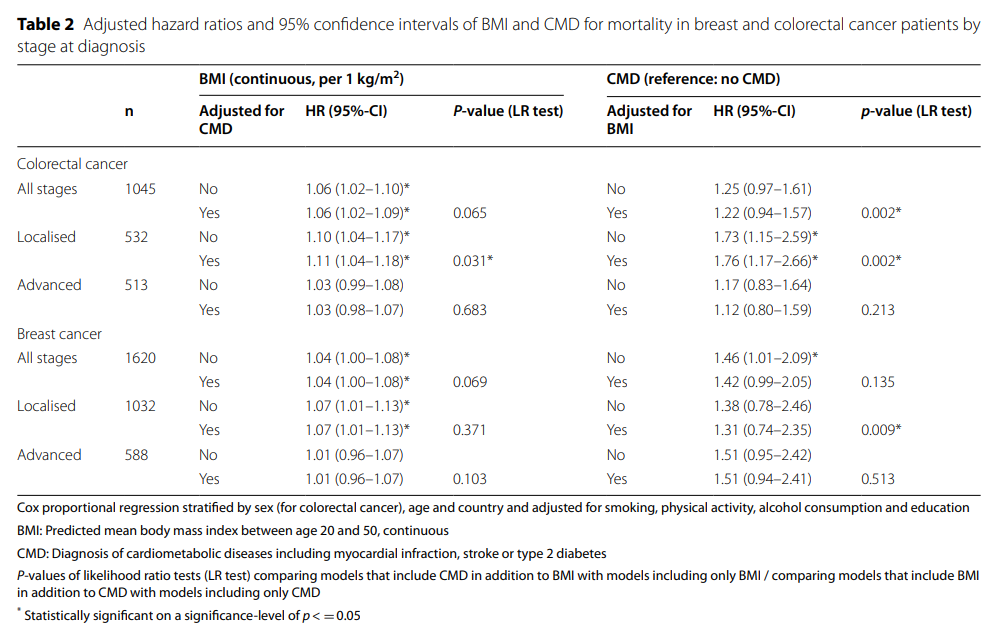

In all stages of colorectal cancer, the survival risk ratio of CMD to non CMD was 1.25, but the confidence interval included 0. In patients with localized colorectal cancer, CMD was associated with a 73% increase in mortality (95% CI 1.15-2.59).
Adjustment for BMI resulted in a slight increase in effect estimates (HR 1.76, 95%ci 1.17-2.66). The HR for survival at unadjusted BMI was 1.17 (95%ci 0.83-1.64) for patients with advanced colorectal cancer with CMD and 1.12 (95%ci 0.80-1.59) for the adjusted model compared with those without CMD.
Likelihood ratio test showed that adding BMI as a covariate to the model containing CMD improved the model fitting of colorectal cancer (P = 0.002) and local phase (P = 0.002) in the total sample. Adding CMD to the model, the BMI improved model was suitable for local colorectal cancer (P = 0.03).
Breast cancer
In patients with breast cancer, higher mean BMI (per 1 kg/m2 increase) was associated with a 4% increase in the risk of death (Table 2, figure 2). For colorectal cancer, subgroup analysis by disease stage at diagnosis showed a stronger association between BMI and mortality in patients with localized breast cancer. Higher mean BMI was associated with a 7% increase in mortality from localized breast cancer (95%ci for HR 1.01-1.13), while the association with patients with advanced disease was close to zero. After additional adjustment of CMD, the estimated value and confidence interval of BMI effect remained similar.
The presence of CMD increased the risk of death in the total sample of patients with breast cancer (HR 1.46, 95% CI 1.01 – 2.09). In the subgroup analysis by stage, the estimates were very similar, but the confidence interval included zero with / without additional BMI adjustment.
Likelihood ratio test showed that BMI was added as a covariate to the model containing the improved CMD model to fit local breast cancer (P = 0.009).
Cumulative exposure to higher BMI levels in early to middle adulthood (20 to 50 years of age) is associated with poor survival in patients with breast cancer and colorectal cancer, especially for localized diseases, and is not associated with CMD before cancer diagnosis. The history of CMD at the time of cancer diagnosis was in turn associated with poor survival in patients with localized colorectal cancer, and was also not associated with BMI. In the stage specific analysis, the correlation between CMD and survival rate of breast cancer was not significant. These results suggest that BMI has a direct impact on cancer survival, but is not mediated by pre diagnosis CMD, which may help to improve the prognostic stratification of cancer patients affected by cardiac metabolic complications.
Original source:
Kohls, Mirjam et al. “Impact of cumulative body mass index and cardiometabolic diseases on survival among patients with colorectal and breast cancer: a multi-centre cohort study.” BMC Cancer vol. 22 546. 14 May. 2022, doi:10.1186/s12885-022-09589-y.
Article source:
https://www.medsci.cn/article/show_article.do?id=c027e2709822